In my last two posts, I have discussed my heroes at Harvard. There is another personal hero that I should mention, and he also lives in Boston. Dr. William E. Boden is a Professor of Medicine at Boston University School of Medicine and a Lecturer in Medicine at Harvard Medical School. He is the Physician Research Lead for the New England VA Healthcare System and Scientific Director of the Clinical Trials Network.
Dr. Boden first came to my attention as the lead author on the landmark COURAGE trial that proved best practice medical treatment or optimal medical therapy (OMT) alone is as effective as optimal medical therapy plus heart artery stents. In a clinical trial, the lead author is typically the individual who made the most significant intellectual and practical contributions to the research, including writing and editing the manuscript. The COURAGE trial proved that stents added to OMT did nothing to prevent sudden death or heart attack. That is why Dr. Boden is one of my heroes.
The care for patients with stable heart artery disease in the United States today is neither patient-centered nor appropriate. Unlike my other physician heroes, I have been in touch with Dr. Boden several times. In our most recent encounter, Dr. Boden taught me something very important. I have been focusing on inappropriate stent use. Dr. Boden taught me that it is not a matter of OMT or stents in patients with stable heart artery disease. Many patients will need both. Everyone with stable heart artery disease should be on optimal medical therapy as soon as that diagnosis is made. Stable heart artery disease may be symptomatic or asymptomatic. In symptomatic stable heart artery disease, the classic symptom is chest pain with exertion (exertional angina.) In stable angina, a patient will experience chest pain reliably with the same level of stress. If a person with stable angina has chest pain when they walk uphill for six blocks in the cold, every time they do that they will have chest pain at about that same point. If that changes, and chest pain occurs with less stress, then that is unstable angina.
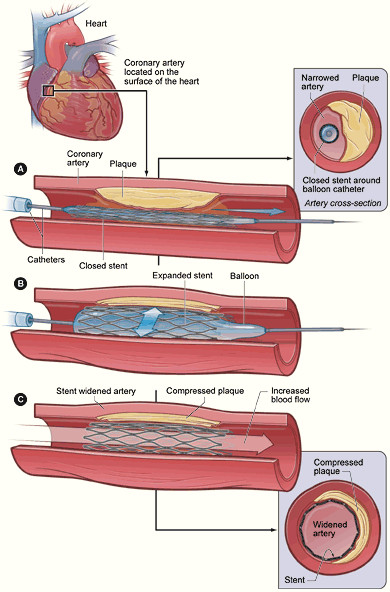
A stent may save your life or prevent a heart attack in unstable angina. Unstable angina means that there is a rupture of inflamed cholesterol deposit that has initiated clot formation. If that clot is partially blocking the artery, that causes a change in the chest pain pattern. If the clot completely blocks the artery, that is a heart attack. It cuts off the supply of oxygen and nutrients downstream and kills the muscle. In unstable angina, opening the clot with a stent and intensifying anticoagulant treatment can prevent a heart attack or save heart muscle.
The COURAGE trial was a landmark study. It answered the question: “Does a stent added to optimal medical therapy reduce death or heart attack compared with optimal medical therapy alone?” It did not. It did produce more benefit in terms of symptom relief, but OMT had benefits there as well. “Rates of angina were consistently lower in the PCI (stent) group than in the medical-therapy group during follow-up, and rates of subsequent revascularization (artery opening) were likewise lower. However, there was a substantial increase in freedom from angina in patients in the medical-therapy group as well, most of which had taken place at 1 year but with a further improvement at 5 years. To what extent this finding reflects a benefit of specific antianginal medications (e.g., nitrates and beta-blockers) or a favorable effect of therapies such as statins on endothelial function and atherosclerosis is unclear.”
There was a substantial reduction in the number of patients with angina (chest pain) in both groups during follow-up. There was a difference in the rates of freedom from angina throughout most of the follow-up period, in favor of the stent group. At 5 years, 74% of patients in the stent group and 72% of those in the medical-therapy group were free of angina. It is that group of about 30% of patients with persistent unacceptable angina or chest pain that would need a stent to improve their quality of life. That is another setting where a stent is appropriate. It is not either or. It is both. It is worth noting that the OMT pioneer Dr. Bernard Lown came to the same conclusion: “Let me repeat. Over any five-year period, we referred less than 30 percent of patients with multi-vessel coronary disease for revascularization.” The key is to use these treatments appropriately. Every patient who wants to live and avoid complications should be on OMT. Going forward, the best hospital systems in the country will have all stable heart artery disease patients on OMT, and they will add stents when appropriate.
Stents are appropriate in patients with unstable angina or a heart attack in progress which together are known as acute coronary syndromes. In acute coronary syndromes stents save heart muscle and lives. Stents are also appropriate in patients with more angina than they want to have despite OMT. Stents in that setting improve the quality of life. That said, most treatment for stable heart artery disease in our country is inappropriate. Most patients are not on OMT, and too many are receiving inappropriate stents. This book is being written to help you know the difference between inappropriate care for heart artery disease and patient-centered appropriate treatment. Make certain that you are on OMT if you have heart artery disease.




Well, the details explain why it was appropriate for me to have stents. I had an acute heart incident going on. And no angina, just bowling ball heaviness in my chest on exercise, and finally congestive heart failure. You actually made me feel guilty for having stents. But I saw the pictures with my own eyes. What a relief because something could finally be done. Life style changes enabled me to exist until that point. I am so happy to have real people I can reach out and touch, explain the need for OMT.
I’ve read about this, and the COURAGE trial, in a number of places over the last year or so. Wish I had known about it 8 years ago, when I had my first 2 stents placed, totally asymptomatic.
It has become so clear that OMT combined with lifestyle changes are a powerful change agent