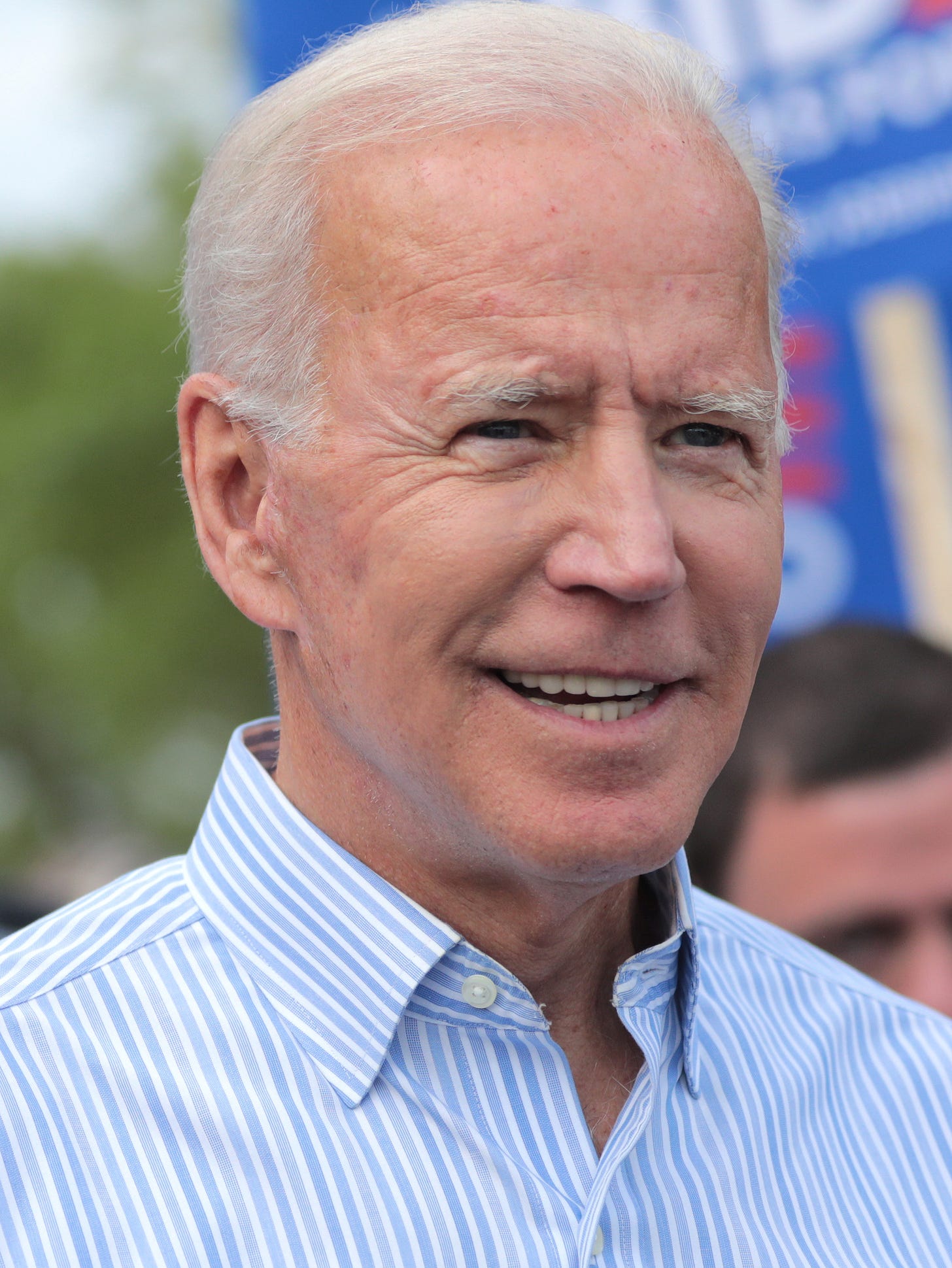
Former President Biden revealed this week that he has a diagnosis of advanced, aggressive prostate cancer that has spread to his bones. I have heard this question asked repeatedly. How could that diagnosis be missed in the president who has an annual physical presumably by the best doctors in the country? That is a very important question and the answer…
Keep reading with a 7-day free trial
Subscribe to Slow Aging and Delay Chronic Disease Development to keep reading this post and get 7 days of free access to the full post archives.